Publisher's note: The author of this post is Katherine Restrepo, who is Health and Human Services Policy Analyst for the Carolina Journal, John Hood Publisher.
RALEIGH — The Raleigh Chamber of Commerce recently sponsored a
health care breakfast panel with three North Carolina hospital CEOs talking about how competition brings out the best in their health systems. Competition is healthy. Competition is a beautiful thing.
The tone of the conversation abruptly changed, however, once the moderator posed a question about the legislature's proposal to relax the state's restrictive certificate-of-need law, which requires medical providers to
ask permission from the state, and then their competitors, before expanding their businesses.
At that point, sponsors already had filed
House Bill 200, which would exempt multi-specialty, same-day surgery centers, formally known as ambulatory surgery centers, from the CON process. The seemingly competitive CEOs were quick to argue that scaling back on CON red tape would put their hospitals at risk.
If more provider-led surgery centers were to break ground, these new facilities could take away the hospitals' most
lucrative outpatient service lines, which they rely on to cover losses incurred from providing required indigent care.
For example, Novant Health's surgery center operates on a 26 percent profit margin. Rex Healthcare, a subsidiary of UNC, projects an impressive 40 percent profit margin for its developing surgery center. 40 percent.
One CEO went on to suggest that relaxing the CON law really just plays to the financial interests of surgeons. Meanwhile, a presentation composed by Carolinas HealthCare System calculates that opening up the health care market to allow for more single-specialty ASCs would benefit a mere 6 percent of specialists.
So much for competition.

What hospitals don't mention is that relaxing CON deals a
huge break to patients, as independent ASCs are typically reimbursed by Medicare
45 percent to 60 percent less for the same procedure compared to those being performed in a hospital outpatient setting. Since
Medicare approved reimbursement for free-standing centers back in 1982, there has been a strong shift to outpatient surgical care. And, thanks to technological innovations, more surgeries are minimally invasive and can be performed safely in these focused factories.
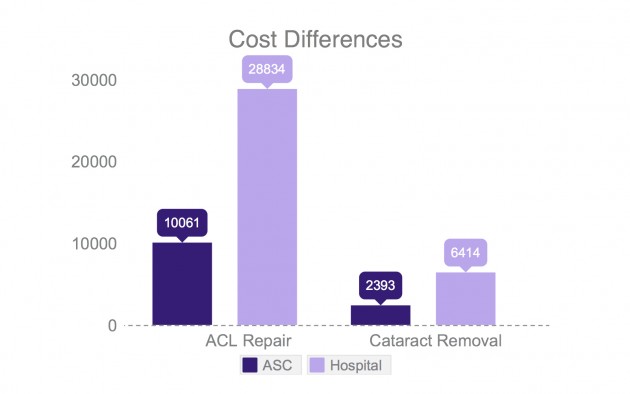
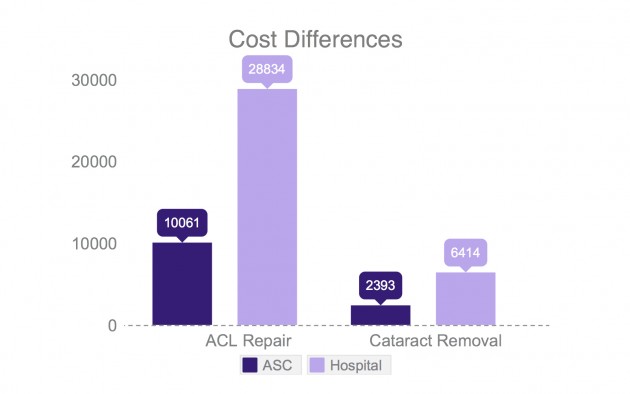
The charts below compare cost differentials of average charges for an ACL repair and a cataract removal — two of the most common outpatient surgeries. These figures are taken from Blue Cross and Blue Shield of North Carolina's publicly accessible
cost estimator tool.
The state's dominant middleman, Blue Cross and Blue Shield, may be sitting on the sidelines with CON reform, but the price transparency tool is providing more ammo for those pushing a long overdue fix to the law. The insurer fears that substantial increases in utilization will outweigh lower health care costs.
Just the opposite transpired since 2005, when CON was loosened to allow for colonoscopies to be performed by gastroenterologists in their own endoscopy units.
Utilization did increase by 28 percent over four years, in part due to the state's baby boomer population, but overall Medicare savings still amounted to over $224 million within six years.
No doubt, outpatient surgery is
big business for hospitals. According to Guy David, associate professor of healthcare management at Wharton School of Business, ambulatory care currently accounts for roughly 60 percent of hospital revenue, up from just 10 percent to 15 percent in the 1990s. Over
70 percent of surgeries in North Carolina and in the U.S. as a whole are performed in some type of outpatient setting — whether it be hospital-affiliated, physician-owned, or a joint venture.
Circling back to House Bill 200, any new ASC, whether provider-led or under hospital ownership, would be required to provide 7 percent charity care. In other words, ASCs need to demonstrate that the combined amount of surgery cases provided to charity care patients plus Medicaid patients is equivalent to at least 7 percent of patient revenue — the value of these cases being based on what Medicare would reimburse.
Aside from three physician-led, single-specialty ASCs having to comply with the 7 percent rule as part of a
demonstration project that began in 2010, there is currently no uniform compliance formula for licensed hospitals in North Carolina to maintain their sales tax, property tax, and income tax-exempt nonprofit status.
The bill also prohibits construction in counties with populations of fewer than 100,000 people, unless the project is approved as a joint venture with a neighboring health system. Rural hospital advocates argue that this concession is necessary to protect suffering community hospitals, but what this ultimately means is that patients in 73 of the 100 counties in the state would not be able to enjoy better access to more affordable health care.

This attempt at reform certainly steps in the right direction toward less regulation and more freedom for providers and patients, yet it's a piecemeal reform. Now that a Senate bill has been filed to
dismantle the law completely, there is an opportunity for the political chess game to be executed in such a way that the Senate will beef up the House version prior to a final deal.